
Abstract
The term depression is used to define the state of a bad mood. In order to diagnose depression, the symptoms of the condition must persist for a period of at least two weeks. Generally, depression is defined as a mental state or a chronic mental disorder that is characterized by a feeling of despair, loneliness, sadness, anhedonia and reduced self-esteem. Depressive disorders are more common for women than men. There are certain hypotheses that indicate the fact that hereditary factors contribute significantly to the development of depression. Needless to say, depressive disorders have been one of the major causes of involuntary admission to the mental hospital. It is estimated by the WHO that about 120 million people in the world suffer from some form of depression yearly. 10% of these are adult citizens of the US above 18 years of age.
The current paper explores the pharmacological effects of anti-depressants in the treatment of depressive and related disorders, including ADHD, OCD, anti-social disorders, eating/sleeping disorders, and clinical depression. The constructivism of this paper lies in its substantial literature review, discussion section, and nursing implication section where the author reveals both the effectiveness and side effects of psychiatric drugs that are used to cure depression. Practical advice of nurses is given for those who work in mental hospitals to reduce side effects and prevent worsening of the patients’ condition.
Depression and related disorders have been treated with the help of a wide variety of medications that are used to salvage the reuptake of neurotransmitters. These neurotransmitters play a key role in stabilizing the excitatory and inhibitory activities at the presynaptic junctions. More importantly, they are all involved in activating neuronal circuits in the human brain and help to transport serotonin and dopamine neurotransmitters between different brain centers. For this reason, it is recommended to use anti-depressants as stimulators of brain activity. Care should be taken during treatment to avoid adverse effects that arise as a result of drug overdose or interaction with other drugs administered concurrently.
Chemically, anti-depressants may differ by the structure of compounds in their atomic nature. For example, there are tricyclic anti-depressants consisting of three atoms and there are also tetracyclic compounds with the four-based compound structure. By effectiveness, selective and serotonin-norepinephrine reuptake inhibitors can be used without the risk of major side effects, when regulated by other medications, and should be used with caution together with other psychic drugs. Noradrenergic and monoamine oxidase inhibitors belong to the new type of psychic drugs that are used in the treatment of depressive disorders. There are specific criteria that have been put in place to diagnose depression. For instance, the ICD 10 stipulates the following:
- Persistence of bad mood and/or loss of interest or pleasure (anhedonia)
- Fatigue or low energy level (anergia)
- Reduced concentration and attention
- Reduced self-esteem and self-confidence
- The feeling of guilt and worthlessness
- Hopelessness about the future
- Intention to commit suicide
- Sleeping disorder
- Reduced appetite
Depressive disorder can be described as mild, moderate or severe depending on the number of symptoms observed. Depressive episodes are also characterized by other symptoms such as amenorrhea, reduced sexual drive/ libido, constipation, and psychomotor retardation. The etiology of depressions is affected by genetic structure, socio-economic factors, health conditions, and cultural background. Genetics: severe forms of depression tend to follow a genetic course more than the less severe forms. As for severe forms, depression is more common for females than males.
Socioeconomic factors such as loss of property, bereavement, and loss of elections can also cause depressive episodes. Health conditions such as HIV and chronic malignancies cause up to 49.27% of depression in the US. Psychiatrists maintain that the patient’s marital status contributes significantly to the development of depression. Single and divorced individuals tend to be more susceptible to depression than those in a stable marriage. Married, divorced and then widowed individuals show a higher incidence of depressive episodes than any other category.
Non-psychiatric conditions such as Addison’s disease, hypogonadism, and Lyme disease tend to cause depressive episodes. Pharmacological treatment of certain conditions such as ischemic heart disease, convulsions, and hypertension contribute significantly to the development of depression.
Discussion
The aim of the current paper is to identify the drugs used in the management of various forms of depression, their mechanism of action including pharmacodynamics and side effects as well as contraindications, nursing implications and the role of a nurse in the treatment care of patients with depressive disorders. In conjunction with the report made by the Centers for Disease Control in 2007, anti-depressant drugs were noted to be the most commonly prescribed drugs according to the survey. The increased use of these drugs is not fully known. However, some specialists have proven that anti-depressants are effective in the treatment of a wide range of conditions such as the Conversion Disorders where psychological stress manifests in physical condition.
The main implications for the use of anti-depressants remain to be major depressive disorders. Major depressive episodes from bipolar disorders to affective/mood disorders have been widely spread in the developed nations. In addition, some chronic illnesses such as heart failure are known to have a strong association with depressive episodes. Treatment of depression is highlighted if it coexists with other medical conditions. This helps to narrow down the prevalence and incidence rates of mortality in chronically ill patients.
Pathophysiology of Depression
The physiology of mood disorders is complicated and inferences are based on brain imaging of the present neurotransmitters in relation to the normal amounts and types of neurotransmitters. In all-purposes, deregulations and imbalances between the levels of norepinephrine and serotonin in the serotonin and dopamine pathways are thought to be the main cause of mood disorders.
In addition to the previously accepted viewpoint that deficient in the number of monoamines in the central chemistry of depression, there exist other endocrine factors. Several hypotheses have been coined to put it simply. Neurotrophic Hypothesis is the main hypothesis that is accepted universally. It states that the nerve growth factors such as the Brain-derived Neurotrophic factor (BDNF) play a significant role in the plasticity and development of the neurons. Depressive episodes are characterized by deficient/degeneration of this factor leading to imbalances between the neurotransmitters. BDNF exerts its effect on the survival value of the neuronal cells by means of activating tyrosine kinase receptor B in neuro-glial cells.
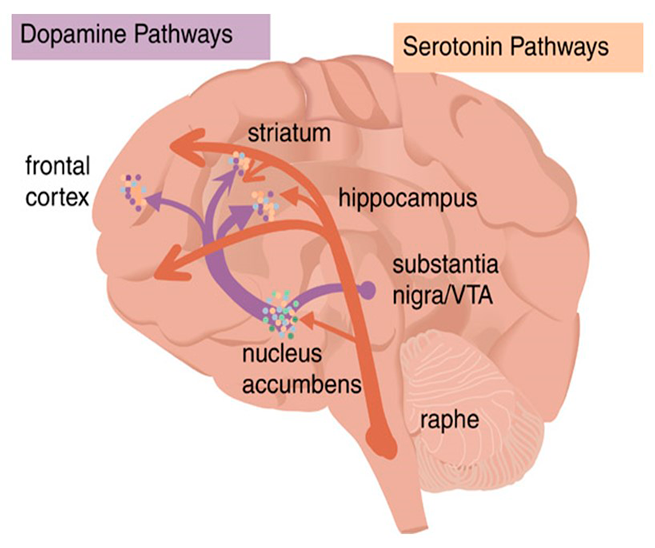
Fig. 1.
Examples of neurotransmitters include the Nor-epinephrine and epinephrine, serotonin and dopamine. Serotonin plays a major role in mood stabilization while dopamine is closely related to the expression of pleasurable emotions.
Investigations and diagnosis of depression are represented by self-report screening questionnaires such as the Beck Depression Inventory (BDI) and the Patient Health Questionnaire (PHQ).
Management of Depression
The management of depressive disorders starts with early detection and effective treatment. There are different ways to manage depression. They entail non-pharmacological and pharmacological treatment. The non-pharmacological ways of treatment include cognitive behavioral therapy, interpersonal therapy, and even electrical convulsion therapy. The aspects of pharmacological treatment are especially important for the current study.
Drug Treatment
There are five categories of anti-depressants, namely:
- Tri-cyclic antidepressants
- Selective Serotonin Reuptake Inhibitors
- Nor-epinephrine and Dopamine Reuptake Inhibitors
- Serotonin and Nor-epinephrine Reuptake Inhibitors
- Mono-amine Oxidase Inhibitors
- Atypical antidepressants
Tri-Cyclic Anti-Depressants. Tricyclic antidepressants such as amitriptyline have been tested both experimentally and clinically since the 1950s. This medication has shown positive results in the treatment of clinical depressive disorders, ADHD, suicide attempts, schizophrenic disorders, and eating disorders. TCAs are considered to have more side effects and therefore SSRI is usually used before TCAs. They are exemplified by desipramine, imipramine, clomipramine, amitriptyline, protriptyline, trimipramine, and doxepin. Amitriptyline is the most commonly used TCA drug. It is used to treat MDD, bipolar disorders, and mood disorders. This medication has also shown positive results in the treatment of clinical depressive disorders, ADHD, suicide attempts, schizophrenic disorders, and eating disorders.
Pharmacokinetics. TCAs are well absorbed and have a long half-life. Medication is given nocturnally since they have a sedating effect. The drugs are metabolized via demethylation, aromatic hydroxylation, and glucuronide conjugation. These drugs are metabolized in the liver by the cytochrome P450 whose 2D6 polymorphism influences the level of conjugation. 5% of the TCAs may pass unmetabolized and excreted via urine. Other TCAs such as desipramine have no known metabolites and their levels of excretion are adversely affected by the concurrent administration of fluoxetine.
Pharmacodynamics. The mechanism of the TCA action is thought to be related mainly to the inhibition of serotonin and norepinephrine reuptake. There is a variation in terms of the affinity of the TCAs towards the inhibition of neurotransmission. For instance, clomipramine reduces the affinity for nor-epinephrine transmission and an increased potential of serotonin affinity. Side effects of TCAs include dry mouth, constipation, and pruritus.
TCAs are contraindicated for patients with conduction disorders, cardiovascular abnormalities, and intolerance to anticholinergic effects of the drugs.
Selective Serotonin Reuptake Inhibitors. They are considered first-line in the treatment of depressive episodes and are used where TCAs are a contraindication. Examples include escitalopram, citalopram, fluoxetine, paroxetine, sertraline, and fluvoxamine. They are used to treat pain such as the neuropathic and fibromyalgia pain. SSRI are also used in the management of generalized anxiety disorders and post-menopausal depression.
Pharmacokinetics. Pharmacokinetics is the same as that of TCAs except that fluoxetine exhibits unique characteristics that are not observed in other SSRIs. It is metabolized to nor-fluoxetine the concentration of which is above the levels of the administered fluoxetine. The elimination half-life of the metabolite is three times greater than that of the original drug. It is known that fluoxetine has to be discontinued three to four week before a mono-amine oxidase inhibitor is started. Failure to follow this rule may precipitate serotonin syndrome. Fluoxetine and paroxetine are important inhibitors of cytochrome P450 isoenzyme such as 2D6 leading to diverse drug interactions.
Pharmacodynamics. Extracellular serotonin binds to the receptor and induces conformational changes in the transporter. As a result, serotonin, sodium, and chloride ions are moved intracellularly. Binding of potassium thus results in the reversion of conformation leading to the release of serotonin within the cell. SSRIs allosterically obstruct the transporter when they directly bind onto the receptor instead of the active sites of serotonin. The common side effects of SSRI include decreased sexual desire and delayed orgasm. Other side effects include anxiety, agitation, nausea, diarrhea, and pseudoparkinsonism.
Serotonin-Norepinephrine Reuptake Inhibitors. Such inhibitors bind on to both serotonin and nor-adrenaline transporters. Examples include duloxetine and venlafaxine. Duloxetine acts as an SSRI in low doses and as SNRI in high doses. They are indicative of major depressive episodes and anxiety disorders. They differ from TCAs by the fact that they lack the antihistamine, antiadrenergic and anticholinergic effect of tetracyclines.
Pharmacokinetics. They are metabolized in the liver by CYP 450 2D6. Unlike other SNRIs, desvenlafaxine is conjugated into a more active form. The half-life of all the SNRIs is about 11 hours. They are transported as free molecules instead of being protein bound. Elimination is via urine.
Pharmacodynamics. They are known to have nor-adrenergic effects. Venlafaxine is a weak inhibitor of norepinephrine transporter, while desvenlafaxine, duloxetine, and milnacipran exhibit equal activities of norepinephrine and serotonin transporter inhibition. The side effects of SNRIs include gastrointestinal disturbances, nausea, and diarrhea.
Mono-amine Oxidase Inhibitors. They interact with several drugs (thus raising the blood pressure) and food that contains amines causing severe hypertension and therefore only used when other drugs fail. There are two types of Monoamine Oxidase Inhibitors. Type A MAOI that is preferable oxidizes serotonin, while type B MAOI metabolizes dopamine. Inhibition of Monoamine Oxidase A is known to have an anti-depressive effect. Examples of MAOI type A and B include phenelzine and tranylcypromine. They inhibit MAO reversibly. Selegiline is a selective MAO B inhibitor that is used for the treatment of Parkinson disease.
Pharmacokinetics. They are readily absorbed in the gastrointestinal tract. Hydrazide inhibitors such as phenelzine are acetylated in the liver and manifestation of the drug persists long after the drug has been eliminated. It is thus not helpful to monitor the half-life of the drug in relation to the patient’s status.
Pharmacodynamics. They inhibit MAO thus increasing the levels of tyramine. Tyramine increases the release of norepinephrine from the terminals. Cheese reaction arises when MAOI are used together with cheese containing foods. This leads to cardiac arrhythmias that may cost the patient’s life. Tranylcypromine is more potent than phenelzine. In addition to MAOI, it increases the release of norepinephrine and serotonin from presynaptic nerve terminals.
Adverse effects of MAOI include drowsiness, dry mouth, weight gain, postural hypotension, sexual disturbances, and headache.
Norepinephrine and Dopamine Reuptake Inhibitors. Bupropion, also known as Wellbutrin, falls into this category. It is among the few antidepressants with no sexual dysfunction as a side effect. However, continuous use of the drug predisposes the patient to seizures.
This drug functions by increasing the levels of NE and dopamine. Side effects include myoclonic seizures, tremors, nausea, and vomiting.
Atypical Antidepressants. These do not fit precisely into any antidepressant category. The category includes; trazodone (Oleptro) and mirtazapine (Remeron). The newest medication in this class of drugs is vilazodone (Viibryd).it has the lowest risk of sexual side effects.
Generally, antidepressants are widely used. They are used in the management of eating disorders such as anorexia nervosa and bulimia nervosa. Smoking cessation, premenstrual dysphoric disorders, and anxiety disorders are also indication result of the use of antidepressants.
Other drugs such as Lithium are used in the management of bipolar disorders. However, the drug is replaced by antipsychotics due to its narrow therapeutic index of 0.6 to 1.2 mg. Outside the dosage range, lithium causes adverse effects.
Unlabelled Uses of Antidepressants
Fluoxetine is used in the management of Raynaud’s phenomenon, fibromyalgia, hot flushes, and diabetic neuropathy. Citalopram is used for the treatment of the premenstrual disorder, anorexia and bulimia nervosa, and pathological gambling. Paroxetine is used for the treatment of pruritus and stuttering. Bupropion is effective in the treatment of neuropathic pain and ADHD. TCAs are used to treat irritable bowel disease. Trazadone are used in the management of insomnia and cocaine withdrawal.
Nursing Implications
The nurse has a major role to play in the management of patients with depressive disorders. To begin with, the nurse has to ensure that the patient receives medication according to the doctor’s prescription. This entails dosage and frequency of the drug’s use. The prognosis of the patient’s condition usually represents a report that should be at the nurse’s finger-tips. Any side effects of the drugs that may overwhelm the patient should be reported to the doctor in good time for an early change of regimen. The elimination of the symptoms of depression should be monitored so as to avoid overstaying of the patient in the ward. The nurse also encourages the patient and assesses the possibility of developing suicidal thoughts for adequate intervention.
Anti-depressants have been the most commonly used medication for many years due to the increased incidences of psychiatric cases such as mood disorders, Attention Deficit Hyperactive Disorders, bipolar disorders, and major depressing disorders. Secondary depression should be managed along with the definitive treatment of the comorbid condition. The readers of the current paper are required to understand what depression is, the development of this condition, its pathophysiology, and different drugs used for the management of depression.
It is worth noting that due to the side effects of medications, some of the antidepressants should be avoided or used with the extra care due to frequent consequences in patients with high risks for the heart failure, insomnia, eating/sleeping disorders, heart arrhythmia, stomach neurotic pain, and sexual dysfunction.













